Alcohol withdrawal syndrome is a potentially life-threatening condition that can occur in people who have been drinking heavily for weeks, months, or years and then either stop or significantly reduce their alcohol consumption.

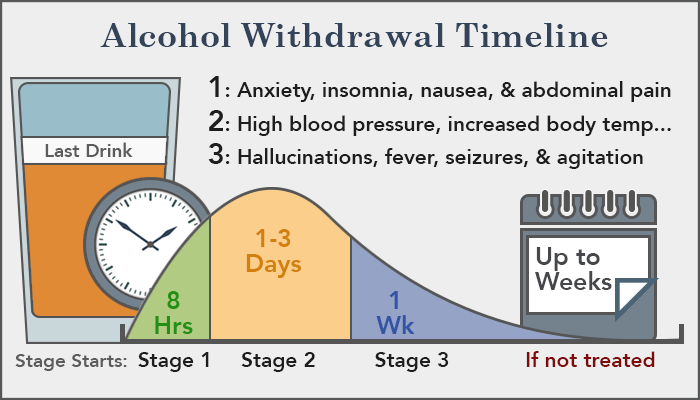
Alcohol withdrawal symptoms can begin as early as two hours after the last drink, persist for weeks, and range from mild anxiety and shakiness to severe complications, such as seizures and delirium tremens (also called DTs). The death rate from DTs — which are characterized by confusion, rapid heartbeat, and fever — is estimated to range from 1% to 5%.
If you have mild to moderate withdrawal symptoms, your doctor may prefer to treat you in an outpatient setting, especially if you have supportive family and friends. Outpatient detoxification is safe, effective, and less costly than inpatient detoxification at a hospital or other facility.
However, you may require inpatient treatment if you don’t have a reliable social network, are pregnant, or have a history of any of the following:
Severe withdrawal symptoms
Withdrawal seizures or DTs
Multiple previous detoxifications
Certain medical or psychiatric illnesses
The goals of treatment are threefold: reducing immediate withdrawal symptoms, preventing complications, and beginning long-term therapy to promote alcohol abstinence.
Alcohol Withdrawal Symptoms
- If you are dependent on alcohol, you may experience any of these common and less severe withdrawal symptoms as early as 6 hours after your last intake of alcohol:
- Insomnia.
- Anxiety.
- Headache.
- Gastrointestinal disturbances.
- Palpitations (rapid, irregular heart beats).
- Sweating.
Theoretically, gabapentin’s ability to increase GABA production may be responsible for producing a calming effect on a number of these alcohol withdrawal symptoms.
Research studies have added further insights as to how gabapentin succeeds in relieving a number of these symptoms.
Prescription drugs of choice include benzodiazepines, such asdiazepam (Valium), chlordiazepoxide (Librium), lorazepam (Ativan), andoxazepam (Serax). Such medications can help control the shakiness, anxiety, and confusion associated with alcohol withdrawal and reduce the risk of withdrawal seizures and DTs. In patients with mild to moderate symptoms, the anticonvulsant drug carbamazepine(Tegretol) may be an effective alternative to benzodiazepines, because it is not sedating and has low potential for abuse.
To help manage withdrawal complications, your doctor may consider adding other drugs to a benzodiazepine regimen. These may include:
- An antipsychotic drug, which can help relieve agitation and hallucinations
- A beta-blocker, which may help curb a fast heart rate and elevatedblood pressure related to withdrawal and reduce the strain of alcohol withdrawal in people with coronary artery disease
- Clonidine (Catapres), another blood pressure drug
- Phenytoin (Dilantin), an anticonvulsant which doesn’t treat withdrawal seizures but may be useful in people with an underlying seizure disorder
If you have severe vomiting, seizures or delirium tremens, the safest place for you to be treated is in a hospital. For delirium tremens, treatment in an intensive care unit (ICU) is often required. In an ICU, your heart rate, blood pressure, and breathing can be monitored closely in case emergency life-support (such as artificial breathing by a machine) is needed.
Medicines called benzodiazepines can lessen alcohol withdrawal symptoms. Commonly used medicines in this group include chlordiazepoxide (Librium) and lorazepam (Ativan).
Most alcohol abusers who are having withdrawal symptoms have a shortage of several vitamins and minerals and can benefit from nutritional supplements. In particular, alcohol abuse can create a shortage of folate,thiamine, magnesium, zinc and phosphate. It also can cause low blood sugar.
DETOX AND TREATMENT
Abruptly stopping gabapentin can increase the likelihood of seizures, so it’s important to seek help when looking to quit.4 If you are getting treatment for a gabapentin abuse problem, you will likely start with detox so that you can slowly eliminate the drug from your body in a controlled manner. After completing detox, you will need medical clearance before transitioning into an inpatient or outpatient treatment program. There are a number of gabapentin addiction treatment options available, including:
- Detox: After long or heavy use of gabapentin, your body becomes dependent on the drug and needs it in its system to function and avoid a potentially perilous withdrawal syndrome.Getting medical detox helps you to slowly wean off gabapentin while under medical supervision.
- Inpatient Treatment: If your gabapentin addiction is severe or you have co-occurring mental health or medical issues, an inpatient program can provide you with intensive care. Inpatient treatment requires that you live at the facility for the entire duration of your treatment. These programs provide a high level of structure and a safe environment that minimizes triggers to use gabapentin. Before you begin treatment, medical professionals will assess your situation and your addiction in order to create a tailored treatment plan. This may include individual and group therapy, family counseling, relapse prevention classes, support groups and aftercare planning.
- Residential Treatment: A residential program can provide a high level of care, structured environment, and 24/7 medical monitoring while you treat your gabapentin addiction. If you require a longer stay and intensive services, a residential facility is a great option. There is a wide range of residential programs available, including facilities that offer dual diagnosis treatment, nutritional counseling, family therapy, and aftercare treatment options.
- Outpatient Programs: After completing detox and/or inpatient treatment, you may move on to an outpatient treatment. You might also start in an outpatient program if your addiction hasn’t progressed to the point of requiring intense inpatient care. When youseek treatment on an outpatient basis, you will live at home and visit the facility for a set number of hours per week to work with a therapist and engage in group therapy.
- Support Groups: Before, during, or after treatment, you may attend 12-step meetings like AA/NA or other support groups. When you go to a support group you will be welcomed by people who know what you’ve been through because they’ve gone through it too. Feeling accepted can make a huge difference in your recovery because you will create a new support network of sober individuals and learn from people who have been abstinent from drugs for a longer period of time.
- Aftercare: In rehab, you will prepare for your transition out of treatment by creating an aftercare plan. This will look different for every person and may include transitioning into a sober living facility, locating a counselor or therapist outside of treatment, and regularly attending 12-step meetings or other support groups. After you leave treatment, it is important that you stay involved with some sort of care to prevent relapse.